Customized vascular models tailored for optimal catheter choice: Illustrated in two aneurysm embolization scenarios
In the realm of interventional radiology, a significant breakthrough has been made with the use of 3D printed, patient-specific vascular models. These innovative tools have proven to be instrumental in complex aneurysm coil embolization procedures, offering numerous benefits that enhance precision, safety, and efficacy.
The institutional review board has approved the use of these vascular models for retrospective case reports, such as two recent instances of complex aneurysm coil embolization. These cases highlight the crucial role of these models in catheter selection and the overall success of the procedures.
Enhanced Preoperative Planning and Simulation
These models provide clinicians with a physical replica of the patient's vascular structure, enabling them to simulate the coil embolization procedure. This meticulous planning leads to a better understanding of potential challenges and the refinement of strategies before actual treatment.
Improved Device Selection and Sizing
Tailored 3D models help in selecting the optimal coil size and placement, reducing risks related to device misfit or inadequate aneurysm occlusion.
Risk Reduction and Safety
Simulation on patient-specific models can help minimize intraoperative complications by allowing rehearsal in a risk-free environment. This potentially decreases embolization-related morbidity and improves procedural outcomes.
Training and Education
These models serve as valuable tools for training interventionalists in complex vascular anatomies, enhancing procedural confidence and technical skills without patient risk.
Augmented Visualization
Advances integrating 3D segmentation and augmented reality (AR) with these models enhance visualization of vascular anatomy, potentially aiding navigation and precision during embolization.
In summary, patient-specific 3D printed hollow vascular models improve the precision, safety, and efficacy of complex aneurysm coil embolization by enabling detailed preoperative planning, customized device deployment, and enhanced understanding of individual vascular anatomy. While direct clinical outcome data specific to 3D printed hollow models and coil embolization are limited, analogous benefits are well documented in the use of 3D printed models for aneurysm treatment planning and endovascular device sizing.
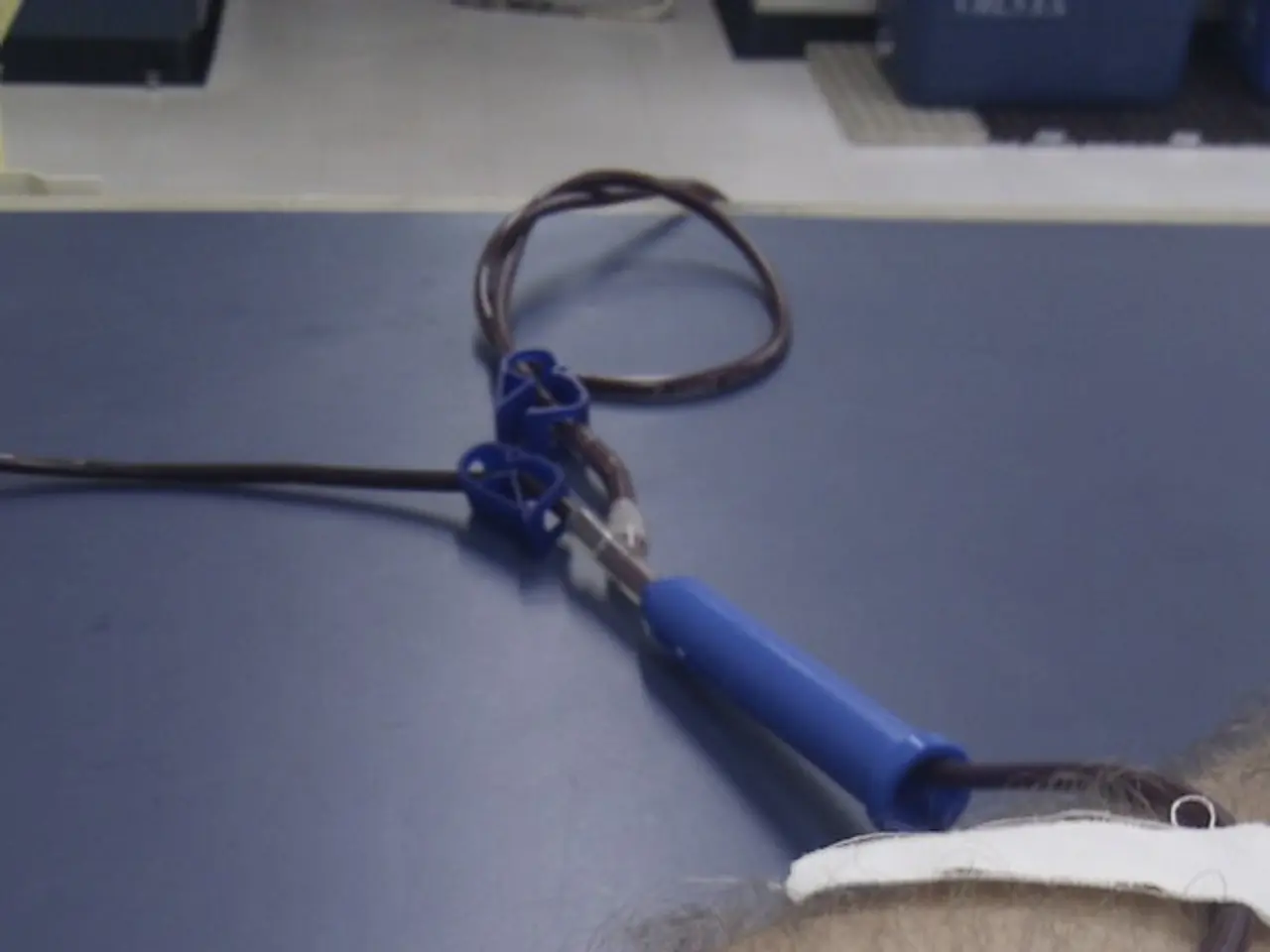
The models are created using digital Imaging and Communications in Medicine (DICOM) data from three-dimensional (3D) computed tomographic angiography (CTA) images, which are then converted to stereolithography (STL) files. The hollow feature of the model is created with a wall thickness of 1.0 mm using MeshMixer. The models are coated with silicone and connected to a sheath in a white box to simulate endovascular procedures without fluoroscopy.
A patient-specific vascular model was created for a female patient in her 40s with a 5 × 5 mm saccular aneurysm at the origin of the dorsal pancreatic artery. Preoperative simulations using this model have been reported to improve embolization material selection and device access, including identifying the most suitable catheter and guidewire. The same catheters were used during the actual procedure, and embolization was successfully completed with no complications.
To address the limitations of existing models, a transparent, flexible, and highly slippery vascular model has been developed. This model accurately reproduces a wide range of vascular structures, providing a more realistic simulation environment.
In conclusion, the use of patient-specific vascular models in complex interventional radiology cases is becoming increasingly important for enhancing preoperative planning, reducing risks, and improving procedural outcomes. These models are set to revolutionize the field of interventional radiology, paving the way for more precise and safer procedures.
- In the field of interventional radiology, the use of science and technology, such as 3D printing, has led to the creation of patient-specific vascular models, which have shown significant benefits in complex aneurysm coil embolization procedures.
- The application of these 3D models extends beyond healthcare procedures, as they are being used for medical-health and wellness, fitness and exercise, cardiovascular health, and even in industries like sports, where understanding complex vascular anatomies would be advantageous.
- The use of these models has also been proposed in sports-betting, as a way to predict outcomes for athletes with certain medical-conditions related to their cardiovascular health or vascular structures.
- As the role of interventional radiology in healthcare continues to evolve, the use of these 3D printed models is poised to revolutionize the field, improving health-and-wellness outcomes, reducing risks, and enhancing precision in various medical procedures.